What is Male Factor Infertility?
Male Factor Infertility refers to cases in which the spermatozoids are either partially or fully responsible for the couple’s infertility. Causes may be genetic or acquired over the male’s lifetime.
At Ginemed, over 50% of males with azoospermia are able to have children using their own sperm. By individually approaching and treating each patient’s unique situation, we are able to obtain spermatozoids even in complicated cases.

Specialised techniques

MACS
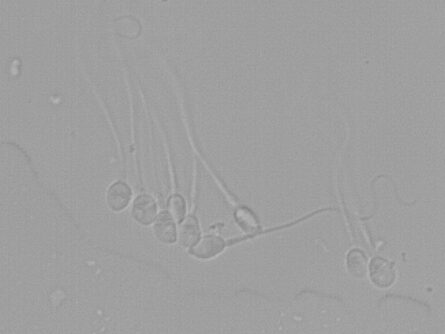
IMSI
Two Fraction Collection System
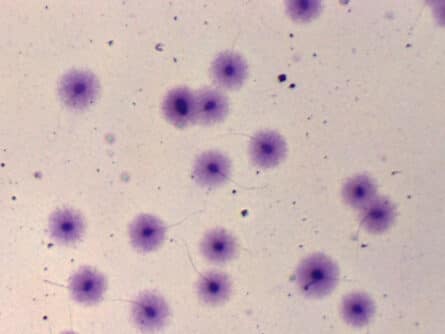
Sperm Fragmentation Test

Testicular Biopsy
Fertile Chip
First fertility visit is free
Request your first appointment cost-free at the clinic closest to you
Frequently asked questions about male factor infertility
- Genetic issues. Male Factor Infertility due to chromosome abnormalities, loss of genetic material or mutations in some of the genes that regulate sperm production.
- Infectious diseases. These can lead to situations such as the destruction of stem cells needed for sperm production, or an inflammatory state which is harmful to sperm.
- Hormone or endocrine disorders. As hormones are responsible for regulating testicular activity, an abnormality could result in fertility issues.
- Immune disorders. These conditions may trigger reactions which attack our tissues, including spermatozoids, or make it difficult for an embryo to be properly recognised during the implantation process.
- Lifestyle and environmental factors. Lifestyle habits and environmental factors can have a negative impact on quantity and quality during the sperm production process.
The tests and exams we request in order to evaluate Male Factor Infertility are:
- Karyotype. This test examines a sample of genetic material to confirm that all chromosomes are correct / complete.
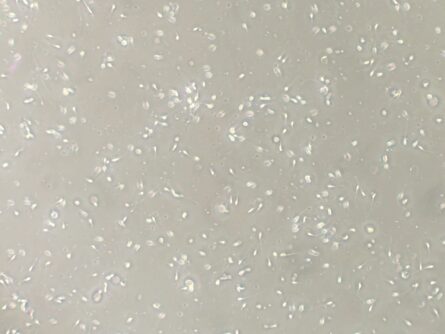
- Sperm Analysis. This analysis studies semen characteristics and provides detailed information on each individual’s natural fertility. A sperm analysis is the main test when it comes to studying male fertility.
- Hormone or endocrine disorders. As hormones are responsible for regulating testicular activity, an abnormality could signify fertility issues.
- Sperm DNA Fragmentation Test. This test is needed to complete the sperm analysis and it informs us about possible sperm DNA damage which cannot be detected through the traditional sperm analysis.
If one of these tests comes back with abnormal results, additional testing will be performed in order to determine the underlying cause of the abnormality: testicular ultrasound, hormone study, sperm culture, FISH sperm analysis, etc.
The treatment prescribed for Male Factor Infertility will depend on the underlying causes:
- Leading a healthy lifestyle is essential. Anything in excess or unhealthy lifestyle choices will have a direct impact on reproduction. In these cases, we generally use supplements or medication that favour sperm formation and protect the sperm from oxidative stress.
- When the cause is a bacterial infection we must treat the patient with antibiotics. The most common are prostate infection and chronic infections. For patients with a prior viral infection which destroyed stem cells, there is no treatment to reverse the damage.
- Hormone disorders should be corrected, if possible, by taking hormones or medication to regulate the issue.
- Varicoceles require surgical management. Surgery is only performed on young males, as the intervention can lead to irreversible damage to the testicle; and on adults when a varicocele is confirmed during a physical examination and the condition also impacts the results of a sperm analysis or sperm DNA fragmentation test.
- When an abnormality is detected in the male’s immune system, medication is prescribed to regulate it.
In addition to these guidelines, males are advised to have frequent ejaculations as this helps to improve sperm quality no matter what the root cause of male infertility is.
At Ginemed, over 50% of patients with azoospermia are able to have children using their own sperm.
Azoospermia is a semen abnormality characterised by the complete absence of spermatozoids in the ejaculate. The causes which lead to obstructive azoospermia are: having undergone a vasectomy, absence of the vas deferens (mutations on the cystic fibrosis gene), and inflammation of the epididymis, among others. Non-obstructive azoospermia, on the other hand, can be caused by: hormone imbalances, genetic disorders or testicular causes triggered by infection or reaction to medications (anabolic steroids, anti-androgen drugs, chemotherapy), among others.
For this reason, the treatment we recommend will depend on the root cause. If azoospermia has resulted from the intake of certain medications, then it will be reversible by stopping the medication. If the root cause is that the male does not produce enough of the hormone FSH, then this hormone will be given to him. For patients with obstructive azoospermia, we can try to fix the blockage through surgical management.
For all other cases, the patient will need to be treated with the help of Assisted Reproduction Techniques. If spermatozoids are found through a testicular biopsy, they can be used to carry out In Vitro Fertilisation (IVF). However, if no sperm are present in the testicular biopsy then the recommendation will be to undergo Assisted Reproduction Treatment using donor sperm.
By individually approaching each patient’s case we are able to obtain spermatozoids in many complex cases.
Although both concepts refer to abnormalities in sperm quality, asthenozoospermia is defined as reduced sperm motility, while teratozoospermia is abnormal sperm morphology.
The term Oligozoospermia is used to describe a low sperm count for males who are in their reproductive years. According to the World Health Organization (WHO), a male who has fewer than 15 million sperm per millilitre of semen is considered to have oligozoospermia.
Hypospermia is a condition in which the male’s ejaculations result in a very low volume of semen, meaning less than 1.5 millilitres. On occasion, a patient may present hypospermia but the amount of spermatozoids is normal. This would mean that there’s an excessive concentration of sperm in the semen sample, causing the individual spermatozoids to bump or crash into each other too often, thus leading to harmful reactions.
However, we need to remember that semen is mainly liquid originating in the prostate and some from the seminal vesicles, while spermatozoids contribute very little to the total volume of the sample.
